Pharmacological Modulation of Long Cardiac QT Interval in Ex Vivo and In Vitro Experimental Models- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF REVIEWS & RESEARCH
Pharmacological Modulation of Long Cardiac QT Interval in Ex Vivo and In Vitro Experimental Models
Authored by Maria Consiglia Trotta
Abstract
Prolongation of cardiac QT interval is one of the
most dangerous consequences of hyperglycemia, acting on accumulation of
reactive oxygen species and impairment of ionic pumps. Previous studies
showed that the selective inhibition of the endogenous aldose reductase 2
(ALR2) activities, responsible of the oxidative heart damage following
diabetes, could be a therapeutic treatment for the high glucose-related
cardiac alterations. Indeed, the newly synthetized ALR2 inhibitor, the
benzofuroxane derivative 5(6)-(benzo[d]thiazol-2-ylmethoxy)benzofuroxane
(BF-5m), dose-dependently reduced the long cardiac QT interval in
isolated rat hearts perfused with high glucose, by increasing in
parallel the expression and activity of endogenous antioxidant pathways
and free radical scavengers such as SIRT1 and its targets MnSOD and
FOXO-1. The reduction of the oxidative stress induced by BF-5m lead also
modifications of the expression of KCNQ1/KCNE1 potassium channels
subunits in H9c2 cardiomyocytes exposed to high glucose, modifying the
expression levels of miR-1, involved in KCNQ1 and KCNE1 expression.
Keywords: Long QT interval; Potassium ion channels; Hyperglycemia; ALR2 inhibition
Abbreviations:
LQTS: Long QT Syndrome; CPCs: Cardiac Progenitor Cells; ALR2- Aldose
Reductase 2; ROS- Reactive Oxygen Species; SDH- Sorbitol Dehydrogenase;
SIRT1- Sirtuinl; TNF-a- Tumor Necrosis Factor Alfa; MnSOD- Manganese
Superoxide-Dismutase; FOXO 1- Forkhead Transcription Factor 1; PKC-
Protein Kinase C
Long QT Interval
Prolongation of cardiac QT interval, characterized by
abnormal QT duration on the surface ECG (higher than 450msec in male
and 470msec in female adults), is an inherited cardiac pathology caused
by disorders of the expression and functionality of cardiac ion channels
[1-3].
About the 90% of Long QT Syndrome (LQTS) cases are related to
alterations of the 3 main genes codifying cardiac sodium and potassium
channels: KCNQ1, KCNH2 and SCN5A genes [4,5].
Mutations in KCNQ1, encoding the a-subunit of the K+ channel Kv7.1,
affect the slow delayed rectifier potassium (IKs) current, creating a
highly arrhythmogenic condition characteristic of the Long QT Syndrome
type 1 (LQTS1), frequently triggered by stress and physical exercise
(above all swimming) [6-8]. Conversely, mutations in KCNH2,
encoding the a-subunit of the K+ channel conducting the IK rectifier
(IKr) current, lead to a reduction in IKr current and are associated to
Long QT Syndrome type 2 (LQTS2) events, occurring during arousal,
especially from auditory stimuli at rest, such as sudden noises and
telephone ringing [8,9]. KCNQ1 and KCNH2
function can be altered also by mutations occurring in genes codifying
their main ancillary single-transmembrane p-subunits, KCNE1 and KCNE2,
encoding the minimal K+ ion channel and the minimal K+ ion channel-
related peptide 1 [9].
Finally, mutations in SCN5A increase the delayed Na+ inward current,
prolonging the action potential duration and are related to Long QT
Syndrome type 3 (LQTS3), occurring in patients asleep or at rest [9,10].
Hyperglycemia Contribution to QT Interval Prolongation
One of the most important risk factor influencing
Long QT prolongation is hyperglycemia: high glucose levels leads to
ventricular instability both in healthy and non diabetic patients and to
significant haemodynamic and electric perturbations in
streptozotocin-diabetic rats, interestingly reversed by the free-
radicals scavenger glutathione [11-14].
Particularly, alterations of IKs current, leading to LQTS1, the most
frequent type of Long QT Syndrome, are strictly related to hyperglycemic
conditions: hyperglycemia, by elevating miR-1/133 expression in cardiac
progenitor cells (CPCs), reduces KCNQ1 and KCNE1 levels, consequently
impairing IKs [15]. Moreover, at level of coronary artery, hyperglycemia down-regulates KV7 potassium channels, influencing their reactivity [16,17].
These studies paved the way to a direct and key role of elevated free
radical production induced by hyperglycemia in potassium channels-linked
QT interval prolongation.
Activation of Aldose Reductase 2 by Hyperglycemia
One of the most important mechanisms through which
hyperglycemia contributes to free radicals induction is the activation
of aldose reductase 2 (ALR2), the first enzyme of the polyol pathway
[18]. While under normoglycemic conditions (3.8-6.1 mmol/L) only about
3% of cellular glucose is converted to s orbital by ALR2, when
hyperglycemic conditions occur (>7 mmol/L) more than 30% of glucose
is shunted to the polyol pathway. This conversion generates reactive
oxygen species (ROS) because ALR2 reduces glucose into s orbital at the
expense of NADPH, essential for generation of the intracellular
antioxidant gluthatione (GSH) [19-21]. Moreover, in the consequent
reactions, the conversion of sorbitol to fructose by sorbitol
dehydrogenase (SDH) depletes the amount of NAD+, an important co-factor
of Sirtuin1 (S1RT1). This deacetylase shows anti-oxidant effects and is
also involved in the regulation of glucose consumption by regulating
insulin expression [22,23].
Aldose Reductase 2 in Diabetes Cardiovascular Diseases
ALR2 plays a critical role in diabetes cardiovascular
complications, as suggested by a number of evidences. ALR2 activation
leads to hyper aggregation of diabetic platelets [18]
and potentially mediates diabetes-induced acceleration of atherogenesis
and endothelial dysfunction in humans, by increasing intracellular
oxidative stress, translocation and phosphorylation of signaling
targets, release of Tumor necrosis factor alfa (TNF-a) and related
cytokines [2426].
Moreover, hyperglycemia-increased ALR2 activity may exacerbate
myocardial dysfunction, inducing cardiac myocyte apoptosis through hyper
osmotic stress and leading to diabetic cardiomyopathy [27].
Hence, the inhibition of ALR2 can prevent or delay the progression of
hyperglycemia-induced cardiovascular diseases. 1n particular, evidences
have shown that the inhibition of ALR2 reduces the detrimental effects
of high glucose levels on the expression of cardiac ion channels KCNQ1/
KCNE1, conducting IKs current and responsible of QT duration.
Aldose Reductase 2 Selective Inhibitors
Since the discovery of ALR2, a huge amount of
experimental data clearly proved the effectiveness of ALR2 inhibitors
(ARls) in treating hyperglycemia-induced pathologies like neuropathy,
nephropathy, retinopathy, and cataract. To date, the main examples of
active compounds undergone clinical trials are spiroderivatives, like
fidarestat and ranirestat; while epalrestat, an acid acetic compound, is
currently marketed for the treatment of diabetic neuropathy,
retinopathy and nephropathy [28-31]. Nonetheless, the development of a number of compounds has been hampered by low in vivo
efficacy and side effects, such as skin reactions or liver toxicity,
some of these were withdrawn from clinical trials; as example, sorbinil,
imirestat and tolrestat were introduced on the market and then
withdrawn [32,33]. Among the chemical entities tested as potential ALR2 inhibitors by Cosconati et al. [34] with few or no side effects, the benzo[c][1.2.5] oxadiazole derivative KM07100 emerged as the most intriguing candidate [34].
This compound is characterized by a core never exploited before and
unpredicted to pose the risk of failure shown by most ARls, because of
either pharmacokinetic restrictions or unwanted side effects. Starting
from the benzo[c] [1.2.5] oxadiazole synthetic precursor, the
benzofuroxane, characterized by nitric oxide (NO) donor, vasorelaxant,
and platelet anti-aggregating activities [35],
a series of novel benzofuroxane derivatives were synthesized fusing the
benzofuroxane ring with aromatic and lipophilic groups [33]. All the synthesized compounds were extensively evaluated by Sartini et al. [33]
for ALR2 inhibitory activity and selectivity, as well as for their
ability to generate NO and efficacy in ROS scavenging. The derivative
5(6)-(benzo[d]thiazol-2-ylmethoxy) benzofuroxane, or from now called
BF-5m, emerged for the excellent correlation between its high ALR2
inhibitory activity and significant NO donor and ROS scavenger, possibly
being a multieffective agent for the treatment of hyperglycemia-induced
QT interval prolongation [33].
BF-5m reduces QT Interval Prolongation by Modifying Cardiac Plasma Membrane KCNQ1 and KCNE1 Levels
Ex vivo and in vitro experimental settings studied the effects of BF-5m in hyperglycemia-induced QT interval prolongation. Di Filippo et al. [36]
showed that in Langendorff's isolated rat hearts, perfused with high
glucose concentration (33mM), BF-5m administration was able to reduce
the prolongation of cardiac QT interval and CPP values induced by
hyperglycemia. Moreover, BF- 5m reduced the structural and functional
cardiac derangement caused by high glucose, by increasing the expression
and activity of the endogenous antioxidant and free radical scavenger
S1RT1. This evidence also confirmed by the increase in the S1RT1 targets
Manganese Superoxide-Dismutase (MnSOD) and in Forkhead transcription
factor 1 (FOXO-1), a transcription factor regulated by S1RT1 and
involved in the modulation of gluconeogenesis, glycogenolysis, and
adipogenesis [37].
These observations were then translated on cultured embryonic rat heart
ventricle H9c2 cells exposed high glucose stimulus, exploring a
possible effect of the decreased ROS levels on Iks current conduction,
responsible of QT interval duration. Trotta et al. [38]
showed for the first time that the blockade of the ALR2 with BF-5m
leads to changes in KCNQ1/KCNE1 potassium channel subunits expression,
during the exposure of H9c2 cells to high glucose. Indeed, BF- 5m
dose-dependently increased plasmatic KCNE1 and KCNQ1 levels and this was
paralleled by a significant down-regulation of miR-1 levels. This
miRNA, showing a higher expression after hyperglycemia stimulation, has
been found to provoke cardiac arrhythmias by altering potassium current
in mature myocytes, reducing he expression of its targets KCNQ1 and
KCNE1 [39].
The ability shown by BF-5m to restore plasmatic KCNE1 and KCNQ1 levels
by up-regulating miR-1 expression is novel evidence, since there was no
correlation linking ALR2 to miR-1 or KCN- potassium channels.
Interestingly, this occurring on the plasma membrane but not on
mitochondrial membrane. This was quite surprising, considering that both
prolongation of cardiac QT interval and hyperglycemia have been
associated to alterations of mitochondrial respiratory chain complex [40,41].
Indeed, under high glucose stimulus, the activation of protein kinase C
(PKC) isoforms induces ALR2 phosphorylation and translocation to the
mitochondria membrane [42,43],
where ALR2 contributes to high glucose-mediated mitochondrial
dysfunction. Moreover, new evidences suggest that after the
translocation on mitochondrial membrane, ALR2 could lead to alterations
of ion channels expression through the phosphorylation and activation of
p53 [44]. This was recently confirmed by Testai et al. [45]
proving that, in line with our evidences, KCNQ4 (or Kv7.4) channels are
the only potassium channels exerting a significant cardioprotective
role in rat cardiac mitochondria against ischemia/ reperfusion. Finally,
the putative preservation of the myocyte normal electrical activity
induced by BF-5m in the in vitro H9c2 setting was also supported
by the improvement of the sharply demarcated and stretched elongated
morphology, characteristic of cardiomyocytes grown in hyperglycemic
conditions and the preservation of the cell biology after BF-5m
exposure.
Conclusion
In conclusion, data from both ex vivo and in vivo
settings suggest that the new aldose ALR2 inhibitor benzofuroxane
derivative BF-5m may supply cardioprotection from high glucose-induced
cardiac QT interval prolongation by reducing the detrimental effects
caused by the oxidative stress on cardiac tissue. Consequently, by
down-regulating miR-1, BF-5m restores plasma membrane KCNE1 and KCNQ1
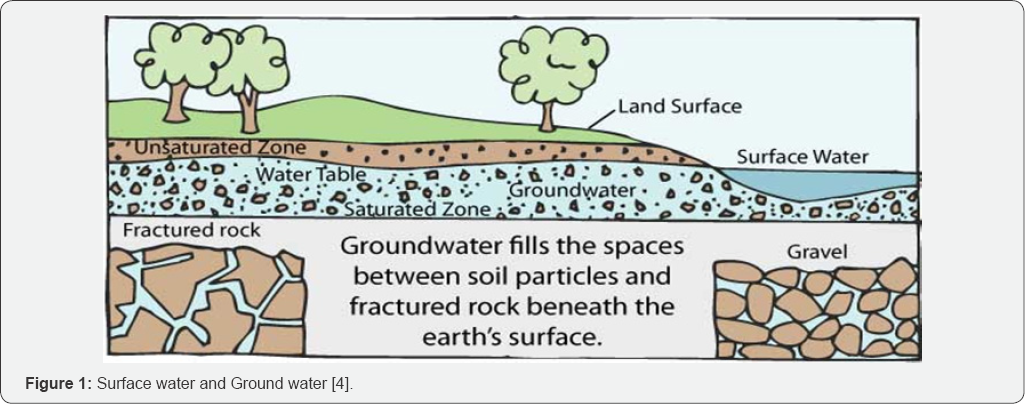
levels, conducting Iks current, responsible of QT interval duration (Figure 1).
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles
in Open Access Journal of
Reviews & Research please click on:
https://juniperpublishers.com/arr/index.php
To know more
about Peer
Review Journal of Reviews & Research click on:
https://juniperpublishers.com/arr/index.php

Comments
Post a Comment