Burden of Non-Communicable Diseases (NCDs): Prevention is better Than Cure- Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF REVIEWS & RESEARCH
Abstract
Non-communicable diseases (NCDs) are the leading
cause of mortality and morbidity worldwide. The harmful use of alcohol,
unhealthy diet, physical inactivity and tobacco use are the leading
modifiable risk factors for NCDs. Unhealthy diet and physical inactivity
contributes to obesity. NCDs are now a major public health concern to
individual quality of life and longevity. The World Health Organization
has set some global strategies giving priorities on increasing
surveillance system, improving public awareness and facilitating quality
of care for chronic diseased cases to reduce the burden of NCDs.
Political commitments to strengthening health systems, effective
interventions, sufficient available resources and health equity are
required to give more focus on preventive and control measures of
non-communicable diseases.
Keywords: NCDs; Chronic disease; Obesity; Primary prevention; Secondary prevention; Health promotion; Health equity
Abbreviations:
NCDs: Non-Communicable Diseases; WHO: World Health Origination; CVD:
Cardiovascular Disease; COPD: Chronic Obstructive Respiratory Disease;
HPV: Human Papilloma Virus
Introduction
Non-communicable diseases (NCDs) are one of the
current threats. By 2030 NCDs are projected to account for more than
75Z% of premature deaths worldwide [1]. WHO defined non-communicable diseases (NCDs) as chronic diseases with prolonged duration and slow progression [2].
The most common non-communicable diseases (NCDs) are cardiovascular
diseases, cancer, chronic respiratory diseases and diabetes. Non-
communicable diseases (NCDs) lead to 70&#xx0025; mortality in most
of the developing countries and cardiovascular diseases are the leading
cause. Smoking, alcohol intake, unhealthy dietary habits and the lack of
physical activity are the major risk factors behind this. Early
detection, Specific treatment as well as creating public awareness are
the key steps to reduce the burden of the non- communicable diseases
(NCDs) [3].
The Risk Factors
The risk factors of non-communicable diseases has been classified into following two categories [4]: (Figure 1).
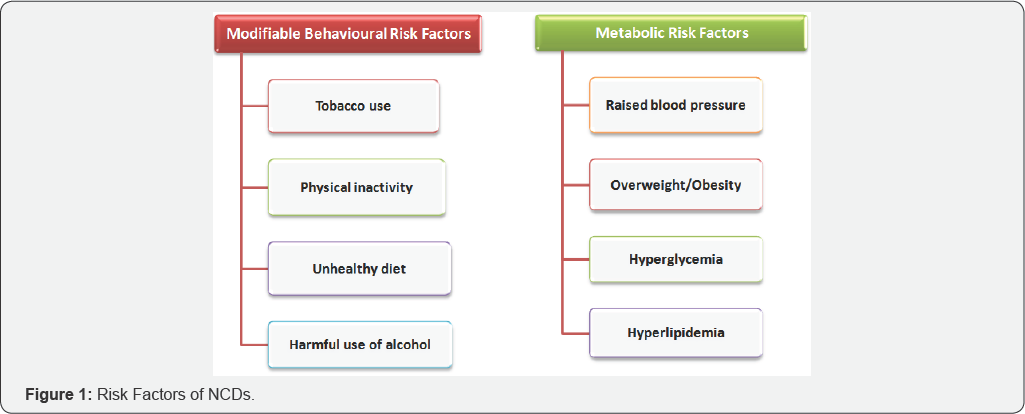
Modifiable risk factors
Modifiable risk factors those behaviors and exposure
that can be changed and which are related to raise a person's risk of
any of the NCDs. The major modifiable risk factors for NCDs include the
followings [4]:
Tobacco use: Tobacco use is one of the major
preventable causes of NCDs which accounts for 7.2 million mortality
every year. Global trends for tobacco consumption are increasing day by
day [5]. WHO projected that by 2020 it will cause around 7.5 million deaths annually [6]. By acting together it is a necessity to take immediate action against tobacco use [7].
Physical inactivity: Inadequate physical
activity is another risk factor for developing major non-communicable
diseases (NCDs) such as coronary heart disease, type 2 diabetes, and
certain cancers [8]. Worldwide in every year about 1.6 million mortality are related to inadequate physical activity [4].
Unhealthy diet: Unhealthy diets are those
diets which contain a high amount of fats, free sugars and salts.
According to WHO about 4.1million annual deaths have been reported due
to excess salt intake [4].
Low intake of fruits and vegetables are associated with
gastrointestinal cancer, coronary heart disease and stroke. Physical
inactivity and unhealthy diets are the leading causes for overweight and
obesity [9].
Excess consumption of saturated fat and trans-fat and high intake of
sugar and salt with low intake of fruits and fresh vegetables
contributes to diet- related NCDs [10].
Harmful intake of alcohol: Uncontrolled
alcohol consumption is associated with adverse health outcomes. Harmful
intake of alcohol is related to develop more than 10&#xx0025;
non-communicable diseases worldwide [11].
Metabolic risk factors
Metabolic risk factors are associated with harmful
biochemical processes in human body that ultimately leads to adverse
health outcomes. The common metabolic risk factors for non-communicable
diseases (NCDs) includes: [4]
Raised blood pressure: Raised blood pressure
is major risk factors for certain cardiovascular diseases such as
coronary heart disease, ischemic heart disease and hemorrhagic shock and
proper maintaining the blood pressure below 140/90mm of Hg can reduce
the risk for any cardiovascular complications [12].
Overweight and obesity: In both developing and
developed countries the prevalence rate of overweight and obesity,
which are considered as the key risk factors for non-communicable
diseases (NCDs) are increasing day by day [13].
Hyperglycemia: Hyperglycemia or high blood glucose levels are one of the clinical features for patient suffering from diabetes mellitus [14].
Several studies showed that mortality rate and substantial neurological
disability after acute stroke are commonly associated with diabetic
patient than non-diabetic one [14-18].
The Four Major Non-Communicable Diseases (NCDs)
Unfortunately most of the communicable diseases are
diagnosed in the advanced stages when the treatment is more costly and
complications are more severe. By early diagnosis and prompt treatment
these non-communicable diseases (NCDs) are preventable and controllable.
According to WHO the major four non-communicable diseases (NCDs) are: [19,20]
Cardiovascular disease (CVD)<
Cardiovascular disease (CVD) is the primary cause of
death globally and in the last century heart disease and stroke became
very common [20].
Cancer: By 2030 there are projected 11 million
cases of cancers will be diagnosed annually in the lower-middle- income
countries. Lung cancer is the number one killer which is associated
with smoking. Other common cancers are colon cancer, uterine cancer etc [20].
Diabetes: Uncontrolled diabetes is associated
with severe consequences like renal failure, stroke, heart disease and
some neurological complications [21].
Chronic Respiratory Diseases: Chronic
respiratory diseases include Chronic obstructive respiratory disease
(COPD) and asthma. The leading cause of Chronic obstructive respiratory
disease (COPD) is smoking. The other causes are air pollution,
occupational dusts and chemicals. COPD is also preventable [19,20].
Disease Prevention
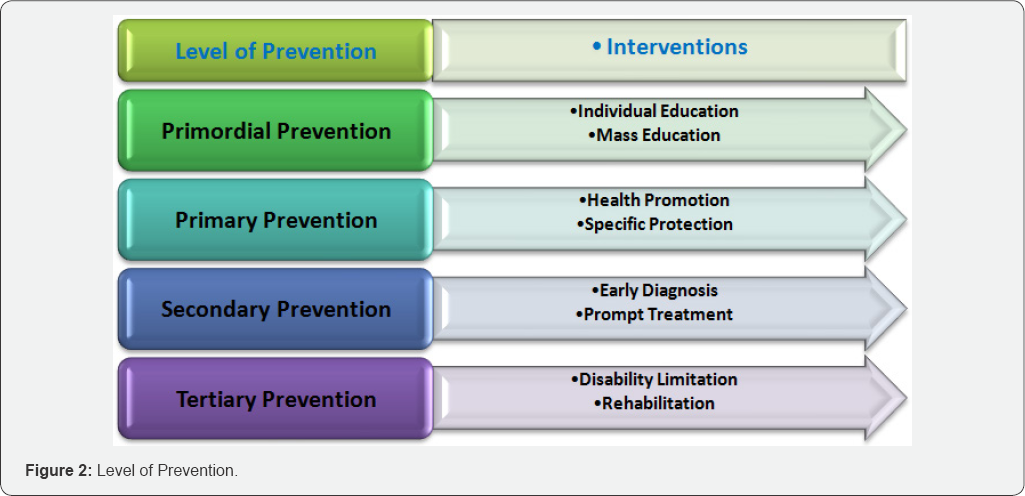
According to WHO the disease prevention can be classified into following four levels: [22]
Primordial prevention<
It includes the actions and measures that inhibit the
emergence of risk factors in the form of environmental, economic,
social, and behavioral conditions and cultural patterns of living. The
main intervention in primordial prevention is through individual and
mass education.
Primary prevention: These preventive measures
are taken for avoiding the manifestation of a disease. The intervention
under primary prevention includes health promotion such as oral &
dental hygiene education and specific protection. Example of specific
protection includes immunization, nutritional and food supplementation
etc.
Secondary prevention: Secondary prevention
undertaken to halt the progress of disease at its earliest stage. Its
intervention includes early diagnosis and prompt treatment of the
diseased condition. The activities under secondary prevention include
population-based screening programmers for early detection of diseases,
provision of chemo-prophylactic agents to control risk factors of
specific non-communicable disease etc.
Tertiary Prevention: The interventions under
the tertiary prevention include disability limitation and
rehabilitation. Disability limitation prevents the occurrence of further
complications, impairments, disabilities and handicaps or even death.
One example for disability limitation is application of plaster cast to a
patient to prevent further disability like malunion or non-union.
Rehabilitation can be medical, vocational, social, emotional or
psychological rehabilitation (Figure 2).
Prevention of Non-Communicable Diseases (NCDs): The Way to Move Forward
In the Global Action Plan for the Prevention and
Control of Non-Communicable diseases, 2013-2020 Guide, WHO has given
some recommendations in the following areas: [23]
Policy
Public awareness and Political commitment: Raising public and political awareness about prevention and control of NCDs
Integrated action: Integration of NCDs into the poverty alleviation strategies.
Capacity-building: Strengthening international
cooperation, capacity-building, health workforce, leadership,
governance, multispectral action and partnerships for prevention and
control of non-communicable diseases.
Effective communications: Effective communications has the key role behind raising public awareness.
Social mobilizations: Social mobilizations are a necessity for prevention and control of NCDs.
Budgetary allocations: It is a requirement to give more focus on budgetary allocations for prevention and control of NCDs.
Development of a national multisectoral policy:
To develop and implement a national multisectoral policy with
multi-stakeholder engagement for the prevention and control of
non-communicable diseases is another key issue.
Tobacco use
Taxation
To reduce the easy accessibility and affordability of tobacco it is mandatory to increase taxation.
Smoke-free environments: It is required to
make policy for creating and maintaining the smoke-free environments in
all indoor workplaces, public places and also public transports.
Public awareness: Public awareness can be increased by effective implementation of different types of health promotion programs.
Banning: One of the effective policies is banning tobacco advertisement.
Harmful use of Alcohol
Public awareness
This can be achieved by encouraging communities for life time modifications.
Political commitment: Effective implementation of political commitment has a crucial role in the reduction of the harmful use of alcohol.
At risk group: Providing early detection and immediate treatment at high risk groups can prevent any associated complications.
Policy: By strengthening and effective
implementation the drink-driving policies and reducing easy
accessibility and availability of alcohol can reduce the harmful effect
of alcohol.
Restriction and Taxation: Restriction in alcohol advertising and increase tax on alcoholic beverages can prevent the easy accessibility of the alcohol.
Unhealthy Diet & Physical Inactivity
Healthy Food
Giving more priorities on fruits and vegetables, less
salt intake and replacing saturated fats with unsaturated fats are the
preliminary step to prevent non-communicable diseases (NCDs).
Supportive Environment: Self and health-oriented environments for physical activity are one of the mandatory conditions for a healthy life.
Marketing of Healthy Foods: By decreasing the
marketing of fast foods or junk foods is one of the fundamental steps to
take prevention at the primordial level. It will help the children to
practice a healthy food habits from their early developmental stages of
life.
Strategy for Infant and Young Child Feeding:
By effective implementation of the WHO global strategy for infant and
young child feeding will ensure all children worldwide a healthy
childhood.
Health Promotion Programs: By implementing
different types of health promotion programs about healthy diet and
physical activity in every community will increase the public awareness
globally.
Food sanitation: By strengthening and proper
maintaining food security and food sanitation and implementing
food-related policy options will promote healthy diet.
Financial Aspect
By integrating very cost-effective non-communicable
disease interventions into the basic primary health care package;
sufficient trained workforce at Primary Health Care level; applying
modern technologies in screening, diagnosis and for the treatment;
availability of essential medicines for treatment of major
non-communicable diseases (NCDs) in both public and private facilities;
strengthening the health care system to identify the risk factors of the
non-communicable diseases (NCDs) at all levels and implementation of
cost-effective treatment modalities for palliative care will help to
fight against non-communicable diseases (NCDs) burden worldwide.
Specific Disease Related
Cardiovascular Disease & Diabetes: Prevention and control of Cardiovascular Disease and diabetes can be achieved by:
Appropriate drug therapies: By prescribing
acetylsalicylic, atenolol and thrombolytic therapy (streptokinase) for
acute myocardial infarction and for congestive cardiac failure with ACE
inhibitor, beta-blocker and diuretics CVD and diabetes can be prevented
and controlled in time.
Counseling: Counseling the individual at risk is the primary step for prevention and control of diabetes and cardiovascular diseases.
Population at risk approach: Application of total risk approach for the purposes of diagnosis, treatment and control of hypertension and diabetes.
Secondary prevention: Secondary prevention of rheumatic fever and rheumatic heart disease through early detection and prompt treatment.
Life time modification: Lifetime modification for type-2 diabetes is essential.
Immunization: Influenza vaccination for diabetic patient is necessary
Pre-conception counseling: Patient with
uncontrolled diabetes are associated with adverse birth outcomes. So the
individual at risk of diabetes are required appropriate preconception
counseling.
Secondary prevention: Secondary prevention of
diabetes mellitus by appropriate drug therapy prescribing
angiotensinconverting enzyme inhibitor to prevent progression of renal
disease.
Tertiary prevention: Tertiary prevention of
diabetes mellitus by detection of diabetic retinopathy followed by
appropriate laser photocoagulation therapy to prevent blindness and
appropriate interventions for foot care.
Cancer
Primary prevention
Primary prevention of liver cancer can be achieved by hepatitis B immunization.
Secondary prevention: Secondary prevention of
cervical cancer can be achieved by screening either by cervical cytology
or visual inspection with acetic acid.
Immunization: Vaccination against human papilloma virus (HPV) can reduce the risk of cervical cancer
Population-based screening: Population based
colorectal cancer screening is associated with timely treatment.
Screening by mammography at high risk group can reduce the mortality
rate of breast cancer
Chronic Respiratory Diseases
Cost-effective interventions
Cost-effective interventions are a requirement to reduce indoor air pollution and to prevent occupational lung diseases.
WHO guidelines: Appropriate use of the guidelines of WHO for treatment of asthma can reduce the further complications.
Immunizations: Influenza vaccination for patient with chronic obstructive pulmonary disease can reduce the mortality rates.
Conclusion
Some countries have already given priority to health
equity to improve health for all. To reach the goal it should require
proper implementation of effective strategic objectives, to be
innovative, willing to learn from each other and to build the capacity
by collaborative partnerships and networks. It is mandatory for every
country to put NCDs in their social and economic development plans and
here political supports are more crucial. Commitments to strengthening
health systems are the essential key issue. For effective prevention and
control of non-communicable disease most of the developing countries
required technical expertise and resources from various disciplines. It
is mandatory to limit the exposure of children to food and non-alcoholic
beverage marketing. NCDs prevention and control can be achieved by
multisectoral and multistakeholder initiatives and multilateral
environment agreements that can lead to coordinated action.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open
Access Journal of Reviews & Research please click on:
https://juniperpublishers.com/arr/index.php
https://juniperpublishers.com/arr/index.php
To know more about Open
Access Journals please click on: https://juniperpublishers.com/index.php

Comments
Post a Comment