Bilateral Herpes Simplex Keratitis Presenting as Bilateral Ulcerative Blepharo-Keratoconjunctivitis: A Rarity or Pattern- Juniper Publishers
Bilateral Herpes Simplex Keratitis Presenting as Bilateral Ulcerative Blepharo-Keratoconjunctivitis: A Rarity or Pattern- Juniper Publishers
Authored by CharlesS Zwerling
We report a case of an immunocompetent 77-year-old Caucasian female presenting with bilateral herpes simplex keratitis masquerading as bilateral ulcerative blepharo-keratoconjunctivitis. Most cases of herpes simplex keratitis present unilaterally and uncommon occurrences of bilateral cases range from 1.3% to 10.9%. In literature, bilateral herpes simplex keratitis has been reported for patients with atopic disease, corticosteroid use, autoimmune diseases, and UV A light exposure. Our patient had none of these conditions, but she did suffer from type 2 diabetes mellitus that was well-controlled. She had no prior history of known herpes simplex disease and tested negative for COVID 19. To date, this is the third reported bilateral herpes simplex keratitis case and the second reported in an elderly patient with shared history of prostaglandin usage and presence of diabetes mellitus. Our rationale for reporting this case is that while it seems to be a rare presentation it could be establishing a pattern. The study explores the relationship between a prostaglandin and HSV activation that may allow viral entrance due to epithelial breakdown. Since our patient did not have any of the previously reported immunocompromised states that have been associated with bilateral herpes keratitis, this case may represent a new pattern for HSV infection. Our clinical methods indicate that close follow-up was crucial to identifying the patient’s eye condition as a bilateral herpes simplex keratitis. Due to this potential pattern of disease, a revised management approach may benefit similar patients by selecting alternative treatments for glaucoma early in the disease presentation.
Keywords:Herpes simplex; Dendrite; Corneal ulcer; Blepharo-keratoconjuncitivitis; Peripheral ulcerative keratitis; Prostaglandin
Abbreviations:HSK: Herpes Simplex Keratitis; PCR: Polymerase Chain Reaction
Introduction
The purpose of this paper is to report a rare case of bilateral Herpes simplex keratitis (HSK) masquerading as bilateral ulcerative blepharo-keratoconjunctivitis and consider a potential pattern of disease between herpes simplex keratitis and prostaglandin use. The Herpes simplex virus is a linear double-stranded DNA virus that is an Alphaherpesvirinae member of the Herpesviridae family. While the virus can infect any part of the body, it commonly infects the mouth, genitals and eyes. Ocular herpes can be caused by both HSV-1 and HSV-2 but HSV-1 is the most common etiology. Each year, there are close to 50,000 new and recurring cases of ocular HSV (predominantly type 1) [1]. Approximately 500,000 people in the United States have ocular HSV and the cost for treatment of new and recurrent cases is US $17.7 million per year [2]. HSV is a neurotrophic virus meaning that it can remain latent in sensory and autonomic ganglia where it can reactivate for the lifetime of the host. While herpes simplex virus accounts for many types of ocular diseases, the most common infectious cause of blindness in developed nations is herpetic keratitis, an infection of the cornea. Transmission of HSV-1 is through direct contact of oral secretions or skin sores. Typically, HSV Keratitis is a reactivation of a dormant HSV-1 infection. Like herpetic cold sores, reactivation tends to occur most often during times of emotional or physical stress and especially in immune-incompetent hosts. Recurrent or untreated HSV keratitis may cause corneal scarring, meta=herpetic and neurotropic ulcers. Presentation of HSV is clinically unilateral and in rare cases of the immunocompromised a bilateral presentation may occur. Treatment usually involves topical anti-viral medications. Steroids may be used cautiously in some cases to limit corneal scarring; however, with neuroptic ulcer formation there is a risk for corneal melting and perforation. Frequent follow-up and compliance with medication regimens is crucial. Diagnosis, treatment and follow-up recommendations have been discussed with the patient including surgical intervention with aminograft [3].
Materials and Methods
Initial Presentation of bilateral kerato-conjunctivitis
On May 4, 2020 a 77-year-old white female presented to Goldsboro Eye Clinic with a 4-day history of red painful eyes with markedly decreased vision bilaterally. The patient self-treated with over the counter allergy eye drops without improvement. She denied any itching or allergy type symptoms. Her eye history includes chronic open angle glaucoma under control with Travatan Z and previous history of bilateral diabetic retinopathy managed with focal laser treatment. She has been a well-controlled Type II diabetic with hypertension with no other systemic illness or disease. On examination her best visual acuity was 20/400 OU. IOP was deferred due to the marked keratitis. External exam revealed marked bilateral blepharitis of the lower eye lids. Slit lamp exam demonstrated bilateral limbal ulcerative defects with significant corneal edema and +3 conjunctival injection. There appeared to be no cells or flare in the anterior chamber and there was mild +1 nuclear sclerotic cataracts present. Dilated fundus exam demonstrated mild diabetic retinopathy. Visibility was hindered by the corneal pathology. Treatment plan included topical Tobradex ophthalmic solution every 2 hours, Tobradex ophthalmic ointment at bedtime, and warm compresses. Travatan Z was continued as directed at bedtime. On May 6, 2020 the patient was re-examined with marked improvement in comfort and vision. Her visual acuity had improved to 20/60 OU and IOP readings were 14 and 15. The conjunctival injection had decreased to +2 and the inferior corneal ulceration and secondary corneal edema also improved.
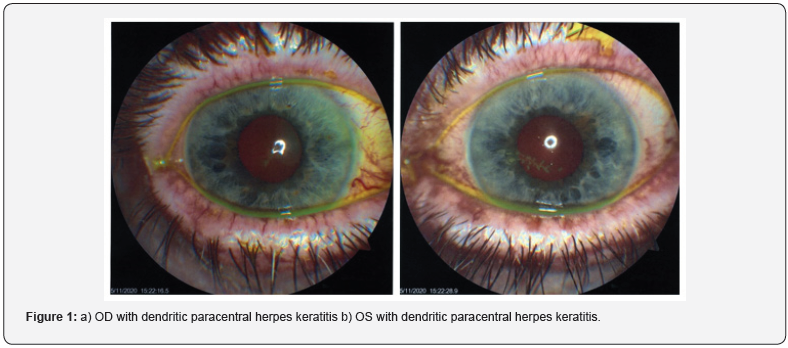
Presence of bilateral dendritic herpes simplex
On May 8, 2020 patient was examined with further visual improvement and comfort. Her vision was 20/50 and 20/40 with IOP measured at 15 and 15. She demonstrated mild paracentral SPK, markedly reduced corneal edema and the presence of dendritic appearing lesions OU at the location of the resolving inferior ulcerative corneal defect with +1 conjunctival inflammation. The patient was asked if she had any recent or current history of URI, oral cold sores and/or fever blisters. She denied any such history. She denied any history of herpetic disease and/or immune problems. As a precaution, blood testing was performed and was negative for ANA. Herpes simplex virus (HSV) antigen was identified in both eyes using polymerase chain reaction (PCR). A COVID 19 test was negative. The patient continued the Tobradex medication and was started on Viroptic 5 times per day and oral Famvir 500mg per day.
On May 11, 2020 the patient was examined with further visual improvement and significant reduction in ocular inflammation. Her vision was 20/40 and 20/30. IOP was 22 and 17. Her conjunctival and eyelid margin inflammation were resolved, and her dendritic lesions demonstrated reduction in size and number. There was minimal corneal edema and no evidence of anterior or posterior segment inflammation. The Tobradex medication was stopped and replaced with Durezol QID OU. She continued the Viroptic 5 times a day and oral Famvir.
On May 14, 2020 the patient’s vision had improved to 20/30OU and IOP was 23 and 17. There was no ocular inflammation. Slit lamp revealed marked reduction of the dendrites in both eyes. The patient was instructed to continue her Viroptic and Famvir and reduce her Durezol to TID OU.
On May 21, 2020 the patient returned for follow-up with no complaints. Her best visual acuity was 20/30OU and IOP was 20 and 15. Slit lamp revealed resolution of all dendrites and signs of mild subepithelial opacities. She was told to reduce her Durezol to BID and reduce her Viroptic to QID OU.
On May 28, 2020 the patient returned with no complaints. Her best visual acuity remained at 20/30OU and IOP was 17 and 19. OU cornea were clear with signs of mild opacity noted at the site of the previous dendritic formations. She was instructed to titrate to discontinue her Durezol and Viroptic over the next week (Figure 1).
Resolution of bilateral herpes simplex
On June 4, 2020 the patient returned for further follow up with no complaints. Her best vision was 20/30OU and IOP was 17 OU. There was no ocular inflammation and slit lamp exam revealed no active corneal lesions with no dye uptake. She was told to discontinue her Famvir and continue her Travatan as usual. On July 14, 2020 the patient returned with no complaints of any eye pain and/or inflammation. Her best vision was 20/40OD and 20/50OS and IOP was 14OU. There was no ocular inflammation and slit lamp exam revealed no active corneal lesions with negative dye uptake at the previous dendritic areas. She was told to finish her Famvir, Viroptic, and continue to use her Travatan.
Re-occurrence of bilateral herpes simplex
On August 24, 2020 the patient returned with a new complaint of bilateral eye pain and redness. Her vision had decreased to 20/70OU and IOP was 13OD and 10OS. Slit lamp exam revealed =3 injection with bilateral dye uptake in a dendritic pattern OS>OD. She was told to stop her Travatan and start Alphagan P BID OU. She was also instructed to resume her Famvir 500mg qd and Viroptic 5X/per day OU medications.
On August 28, 2020 the patient returned with marked improvement. Her vision was 20/50OU and IOP of 17OD and 12OS. Her conjunctival inflammation was <+1OU and there was marked reduction in the keratitis to a few scattered SPK OU. Her Viroptic was reduced to QID OU and she was told to continue her Famvir qd.
Resolution of bilateral herpes simplex
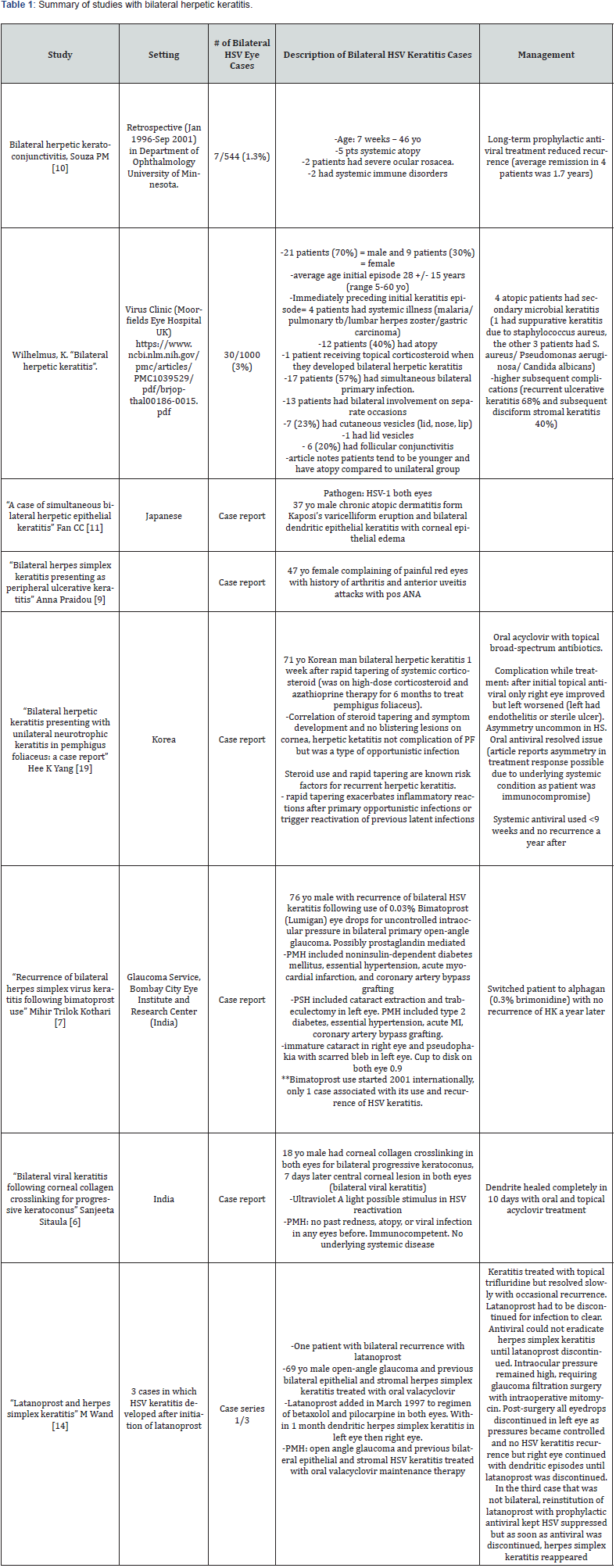
On August 31, 2020 the patient returned with no complaints. Her vision was 20/40OD and 20/50OS. Her IOP was 16OD and 13OS. There was no inflammation and no dye uptake in either eye. She was told to stop her Famvir and Viroptic and continue to use the Alphagan BID OU. On September 8, 2020 the patient returned with no complaints. Her vision was 20/30OD and 20/40OS. IOP was 10OD and 12OS. She was scheduled to return in 3 months or prn (Table 1).
Discussion
HSV keratitis can be divided into two major types: epithelial disease and stromal disease. The epithelial disease is usually due to actively replicating virus while the more common stromal disease is often caused by immunologic mechanisms. A third type, endothelial keratitis, manifests as rejection line-like keratic precipitates and stromal edema [4]. Variations between these subtypes poses a big challenge in accurate diagnoses which is important as treatment methods are very distinct. Usually, herpes simplex keratitis presents unilaterally but bilateral cases have been reported in 1.3% to 10.9% of patients [5]. Bilateral presentation can develop in immunocompromised patients such as those suffering from congenital immune deficiencies, atopy, or long-term immunosuppression [5].
Our case report involved an immunocompetent Type II diabetic elderly patient with bilateral herpes simplex keratitis that presented as bilateral ulcerative blepharo-keratoconjunctivitis. Initially, the patient was treated for a presumed bacterial infection involving her eye lid margins, conjunctiva and cornea. She had no previous history of herpetic infections or symptoms and had a healthy immune system on presentation. Our case is also interesting because most case reports of bilateral herpetic keratitis in immunocompetent individuals have been reported in the young [6]; and without other immunosuppressive diseases besides diabetes in our patient, our case seems to be a rare anomaly for an elderly patient. It could be argued that amidst COVID-19, this patient may have been suffering from the virus mild enough to not recognize any symptoms and this could have created opportunity for HSV-1 to reactivate. This pathophsiology should be considered, since COVID-19 testing has reported a 38% false negative rate for the disease [7]. However, this patient did not have any commonly known COVID-19 symptoms that could be linked with the immunosuppression that could explain bilateral HSV keratitis presentation. For more thorough assessment, a follow-up on COVID-19 antibodies for unusual presentation of COVID-19 would be worth investigating. It would also help challenge any argument for immunosuppression beyond the patient’s established medical conditions. Upon further inspection of our patient’s history, it was acknowledged that the patient was on a prostaglandin analog used for treatment of the patient’s chronic open angle glaucoma. This information is valuable to acknowledge as a possible cause for our patient’s presentation, because there has been another reported case where a 76-year-old male had recurrence of bilateral HSV keratitis following the use of 0.03% Bimatoprost eye drops [8].
Ocular adverse reactions of prostaglandins
The most common adverse reaction observed was ocular hyperemia in 30 to 50% of patients [9]. Up to 3% of patients discontinued therapy due to conjunctival hyperemia9. Mild ocular adverse reactions reported at an incidence of 5 to 10% in clinical studies and included decreased visual acuity, eye discomfort, foreign body sensation, pain and pruritus. More serious ocular adverse reactions reported at an incidence of 1 to 4% in clinical studies included abnormal vision, blepharitis, blurred vision, cataract, conjunctivitis, corneal staining, dry eye, iris discoloration, keratitis, periorbital and lid changes including deepening of the eyelid sulcus, lid margin crusting, ocular inflammation, photophobia, subconjunctival hemorrhage and tearing [9].
Non-ocular adverse reactions of prostaglandins
Non-ocular adverse reactions reported at an incidence of 1 to 5% in these clinical studies were allergy, angina pectoris, anxiety, arthritis, back pain, bradycardia, bronchitis, chest pain, cold/ flu syndrome, depression, dyspepsia, gastrointestinal disorder, headache, hypercholesterolemia, hypertension, hypotension, infection, pain, prostate disorder, sinusitis, urinary incontinence and urinary tract infections [9]. Prostaglandin toxicity studies have widely documented the presence of dry eyes; however in a cross-sectional study, Teresa Rolle et al. [10] noted that tafluprost had no effect on tear stability compared to preservative-free timolol and that the active component of both groups can lead to ocular surface defects [10]. On the other hand, BAK concentrations in prostaglandin preservative solutions have been noted for dry eyes. BAK has been proven to quicken drying of tear film and aggravate preexisting dry eye. This was demonstrated in an openlabel multicentre study with 158 patients where preservative-free tafluprost was better tolerated compared to latanoprost containing preservative solution [11]. It is important to note, however, that a study by Jess T Whitson et al. [12] found no significant difference in tear break-up time and corneal staining among prostaglandins with different BAK concentrations which included bimatoprost (0.005% BAK), latanoprost (0.02% BAK), and travoprost (safZia) [12].
Continuing with the discussion of prostaglandin’s mechanism to causing dry eyes, meibomian gland dysfunction has been an important etiology of dry eye and long-term topical medication of prostaglandins can lead of meibomian gland obstruction [13]. A study done by Luca et al. [14] observed significant morphological changes in meibomian glands through LSCM between preservative and preservative-free prostaglandin groups [14]. These studies lend themselves to suggest that we need a long-term investigation to understand tolerability of the ocular surface in the face of preservatives found in glaucoma medications such as prostaglandin [15-20].
Of note, this patient’s medical history of diabetes mellitus alongside the use of a prostaglandin may have increased her likelihood of presenting with bilateral herpes keratitis. A systemic disease that weakens the immune system allowing for reactivation of the herpes virus and the continuous use of preservativecontaining prostaglandin in this circumstance could have brewed the perfect storm. While our patient presented in May and was being treated accordingly with antivirals, what was most peculiar was her recurrence in late August. When we switched her Alphagan, she rapidly improved in visual acuity and her pressures continued to be maintained. Our case documents one of the few cases documented where this has occurred in a diabetic patient, hence, it would be interesting to gather more data from the collective medical community if more instances have occurred but not documented in case reports. This is important because frequent follow-up of this patient was the key to identifying, modifying the treatment path, and resolving the disease of this patient [20-23].
Conclusion
Bilateral herpetic keratitis masquerading as a bilateral
ulcerative blepharo-keratoconjuncitivitis is a rare presentation
of herpetic disease. With no steroid use, atopic disease, COVID-19
infection, or recent immunosuppressive procedures, our case
presents a rarity of reported for bilateral herpes simplex 1
reactivation and subsequent keratitis. Bilateral herpes simplex
keratitis can pose a diagnostic dilemma in cases with a healthy
immune system and no other systemic symptoms. Excluding
other infectious agents is mandatory for appropriate treatment.
Moreover, this case clearly established a causal relationship with
topical prostaglandin use. Once the prostaglandin was removed,
there was no reoccurrence. Additionally, the most important
aspect to management of patients with rare disease occurrences
is follow-up.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/aboutus.php
For more articles in Open
Access Journal of Reviews & Research please click on:
https://juniperpublishers.com/arr/index.php


Comments
Post a Comment