Causal Relationship Between Chronic Upper Respiratory Infections and Benign Enlargement of Subarachnoid Spaces- Juniper Publishers
Juniper Publishers- Open Access Journal of Annals of Reviews & Research
Causal Relationship Between Chronic Upper Respiratory Infections and Benign Enlargement of Subarachnoid Spaces- Juniper Publishers
Authored by Reagan Collins
Abstract
Benign enlargement of subarachnoid spaces (BESS) is a common clinical finding in pediatric patients. Although a few causes have been put forward, the etiology of the enlargement is largely unknown. Both chronic upper respiratory infections (URI’s) and cor pulmonale (by means of increased right atrial pressure) can hinder venous drainage contributing to increased cerebrospinal fluid (CSF) volume and elevated intracranial pressure (ICP), thus potentially predisposing a patient to enlargements of their subarachnoid spaces to accommodate for these changes. This study aims to determine if a history of chronic upper respiratory infections and cor pulmonale is correlated to a higher incidence of BESS. Scans and medical records from patients under the age of 2 with either macrocephaly or BESS from 2009-2016 were examined to evaluate this possible association. Incidences of chronic URIs and elevated RAP were statistically significantly higher in the BESS population supporting the proposed aim of the study (p< 0.001). Physicians should consider closely monitoring patients with chronic URIs and cor pulmonale for possible BESS and associated sequelae.
Keywords:Upper respiratory tract infections; Benign enlargement of subarachnoid spaces; Increased ICP; Pediatrics; Pediatric neurosurgery
Abbreviations:BESS: Benign Enlargement of Subarachnoid Spaces; MRI: Magnetic Resonance Imaging; CT: Computerized Tomography; CSF: Cerebrospinal Fluid; ICP: Intracranial Pressure; URI: Upper Respiratory Infection; RAP: Right Atrial Pressure
Introduction
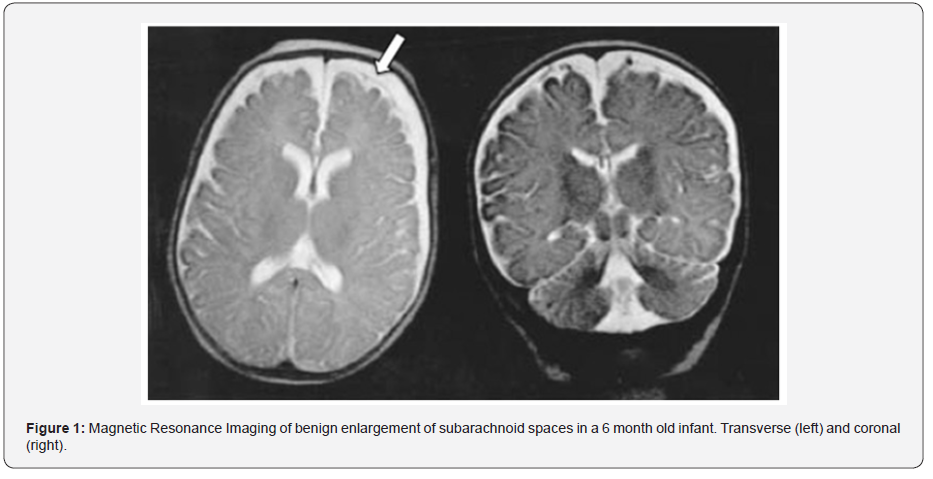
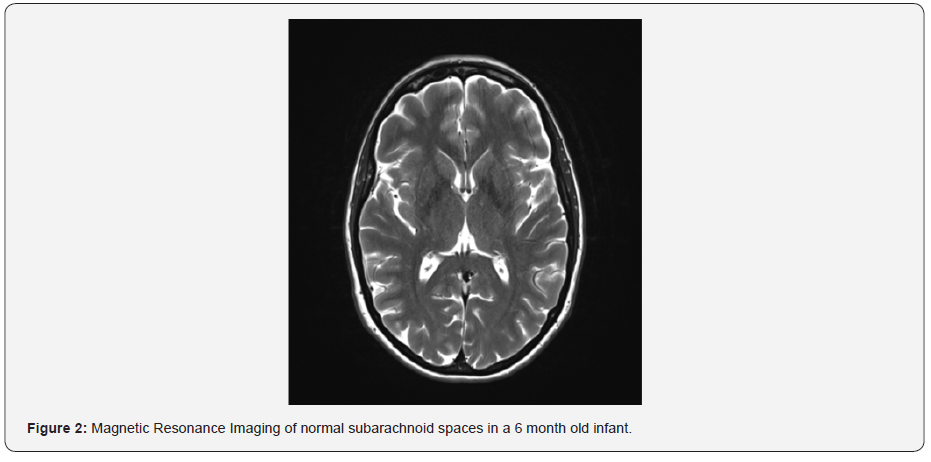
Enlarged subarachnoid spaces in children under the age of two are common and generally considered benign due to stabilization and normalization of the skull closer to and after this time period [1-2]. Typically referred to as BESS (Benign Enlargement of Subarachnoid Spaces), this condition presents after birth and normalizes after age two with little to no complications or neurological deficits (Figure 1 & 2). It does seem to be more common in premature infants than in those who reached full gestation [1-4]. Enlarged subarachnoid spaces are distinguished on magnetic resonance imaging (MRI) and computed tomography (CT) imaging by bifrontal enlargement of subarachnoid space, enlargement of basal cisterns, prominence of cortical sulci, presence of vascular flow-void areas, and their isointense nature as compared to cerebrospinal fluid (CSF) (Figure 1 & 2) [5]. BESS is clinically distinguished by macrocephaly (which has been shown to have a genetic component), bulging or full fontanelles, and increased head circumference [1-4,6]. Though it is generally regarded as benign, patients have an increased risk for developing subdural hemorrhages following minor head trauma and hydrocephaly [7]. Other evidence suggests BESS is correlated with increased incidence of arachnoid cyst formation later in childhood and adulthood [1]. The cause of the condition is largely unknown, and although a few hypotheses have been made as to its origin, there is little consensus in the scientific community.
Following birth, infants are able to accommodate changes in intracranial pressure (ICP) by subtle enlargements of their soft skull and filling of the fontanelles. Symptoms and sequelae of increased ICP include accelerating head circumference, midline shift, papilledema, herniation, and cerebral ischemia, among others [8]. According to the Monro-Kellie Doctrine, an increase in any of the key components (CSF, arterial/venous fluid, and brain parenchyma) can lead to increased ICP in the skull [9]. Subarachnoid spaces house CSF, which is produced by the choroid plexus and absorbed primarily via the dural venous sinuses, along with arachnoid granulations and lymphatics. CSF over-accumulation in the intracranial cavity can be due to abnormal production or resorption, with 90% due to problems with resorption [9]. Chronic upper respiratory infections (URI’s) can cause venous engorgement via compromised expiratory flow, which can unbalance the components within the brain, causing an increase in CSF volume and a rise in ICP [10]. The incidence of respiratory illnesses in the pediatric population is well known to be high, especially in early childhood [11]. Similarly, cor pulmonale secondary to pulmonary hypertension also contributes to venous congestion preventing venous drainage from the head from entering the right atrium and causing imbalances in the key brain components [12]. Based on this knowledge, there is a possibility that BESS could potentially be linked to a prior history of chronic upper respiratory infections or cor pulmonale.
In an adult, an increase in CSF could cause symptoms such as headaches, papilledema, and/or seizures [13]. However, in a child under the age of two, the sutures have yet to fuse and the cranium can enlarge to compensate for the extra CSF without the appearance of any additional symptoms. As pediatric patients age, cranial bones begin to fuse and are therefore less able to accommodate changes in ICP without causing appreciable symptoms [14]. Thus, the risk of experiencing adverse effects of elevated ICP increases with age, so it is important to identify possible predisposing factors such as BESS early in the patient’s life. Our hypothesis is that there is a greater incidence of BESS in children who have a history of elevated right atrial pressure (RAP) caused by URI or cor pulmonale as compared to the general pediatric population. Identifying a correlation between these conditions could potentially help pediatricians watch out for early signs of increased ICP in patients with a history of URI or cor pulmonale and aid in the development of a differential diagnosis.
Materials and Methods
Patients chosen for this retrospective study were all pediatric patients (< 18 years of age) seen for either macrocephaly or BESS before the age of two in the pediatric neurosurgery clinic at either Covenant Women’s and Children’s Hospital or Texas Tech University Health Sciences Center Medical Pavilion from 2009- 2016. The ICD-9 and ICD-10 codes for macrocephaly were used to search the billing database for potential patients. After reviewing all available medical records and scans, only patients without confounding diagnoses and syndromes (e.g. Chiari Malformation) were selected. A chi-squared goodness of fit test examined the statistically significant difference between the incidence of URIs or cor pulmonale in BESS and that of the general pediatric population.
Results
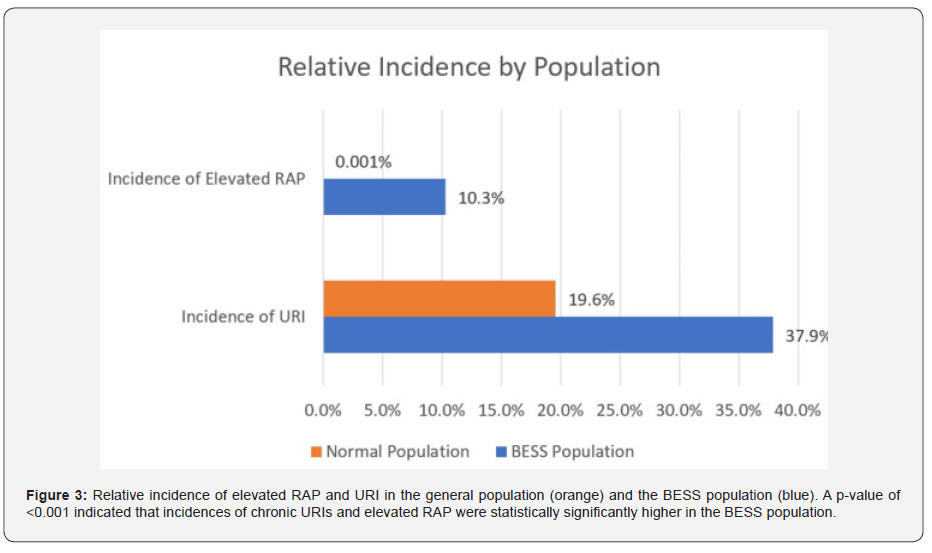
After excluding those with confounding factors such as major gross birth defects or other brain pathology (tumors, Chiari malformation, etc.), 29 patients fit the study criteria. The patients were of varying ethnicities with an overrepresentation of Hispanic and Caucasian patients. Three had cor pulmonale and macrocephaly, 11 had a previous history of chronic URIs and macrocephaly, and 10 had macrocephaly without either preexisting medical condition. The incidence of chronic URIs in pediatric patients under the age of three is 19.6%, while the incidence of right sided heart failure in the general pediatric population is 33.3 per 10,000. Within our sample of macrocephalic patients, the prior incidences of chronic URIs and elevated RAP (cor pulmonale) were 37.9% and 10.3%, respectively, compared to 19.6% and 0.001% in the general population (Figure 3). A p value of < 0.001 indicated that incidences of chronic URIs and elevated RAP were statistically significantly higher in the BESS population. The null hypothesis is rejected in support of the test hypothesis of an increased risk of developing BESS in those patients with a history of cor pulmonale or chronic URIs.
Discussion
While the etiologies of BESS are still unknown, this study presents potential factors leading to the development of BESS. Though it is generally considered a transient condition during normal neurodevelopment, it could also be a result of pathological processes in some children [1]. This information has potential application across a broad variety of healthcare practices. Cranial bone fusion that occurs with aging causes a once distensible calvarium to become rigid and less accommodating to changes in ICP [14]. Given the high incidence of URI in the pediatric population and the relationship this study has established between these infections and the development of BESS, awareness and careful monitoring of young patients with chronic URI and RAP if necessary to prevent possible central nervous system issues. Due to the increased risk of subdural hemorrhage that accompanies BESS, pediatricians might monitor and advise parents on their child’s increased risks for potential hemorrhage with relatively minor trauma, as well as adding a diagnosis to the differential of the etiology of macrocephaly. Particularly for children with a history of chronic URI’s or cor pulmonale, pediatricians should be mindful of the increased risk for BESS and the potential associated comorbidities including increased risk for hemorrhage and cyst formation among other indicated complications. Having a low threshold of suspicion for conditions that lead to elevated ICP in patients with these predisposing conditions could potentially prevent brain injury and preserve CNS functionality by implementing early imaging and treatment. Further research may support the need for these patients to be followed past two years of age for symptoms of increased ICP and cyst formation.
Conclusion
An important application of this knowledge is in the area of child abuse. Child abuse is often high on the differential when a child comes in with subdural hemorrhage because of the necessary force to incur such a bleed in a normal healthy brain. However, that minimum force threshold is lowered in the patients in this study due to increased stretching of the bridging veins. In an area with particularly high rates of child abuse, this could be an important differential diagnosis to consider. With proper patient care and testing, nonaccidental trauma could be ruled out by the patient’s past medical history and scans, as well as situational evidence. Given the high number of URI cases in the pediatric population, recognizing the relationship between these and BESS is an important step in helping physicians provide the best preventative care. BESS, once thought to be completely innocuous, could have some far-reaching consequences for affected children as they get older that have yet to be explored. URIs afflict many pediatric patients, particularly in early childhood. This study has shown that there is a greater incidence of BESS in patients who have experienced chronic URIs and elevated RAP. Therefore, it is important to closely monitor children who suffer from chronic URIs and elevated RAP as they get older to ensure that any sequelae of BESS are swiftly and carefully managed.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/aboutus.php
For more articles in Open
Access Journal of Reviews & Research please click on:
https://juniperpublishers.com/arr/index.php


Comments
Post a Comment